Sitting at her computer one day in late December, Dr. Sarah Osmundson mustered her best argument to approve an abortion for a suffering patient.
The woman was 14 weeks pregnant when she learned her fetus was developing without a skull. This increased the likelihood of a severe buildup of amniotic fluid, which could cause her uterus to rupture and possibly kill her. Osmundson, a maternal-fetal medicine specialist at Vanderbilt University Medical Center who helps patients navigate high-risk pregnancies, knew that outcome was uncommon, but she had seen it happen.
She drafted an email to her colleagues on the Nashville hospital’s abortion committee, arguing that the risk was significant enough to meet the slim exception to Tennessee’s strict abortion ban, which allows termination only when “necessary to prevent the death of the pregnant woman or to prevent serious risk of substantial and irreversible impairment of a major bodily function.” She pleaded with her fellow doctors to spare this woman the gamble when her baby wasn’t even viable.
Then came the replies.
One doctor wasn’t “brave enough.”
Another urged her to consider the optics — approving an abortion in this case could be seen as “cavalier” and trying to circumvent the law. “I’m saying this because I care about you and your personal liberties,” the doctor said.
To Osmundson, the responses reflected just how much abortion bans had warped doctors’ decision-making and forced them to violate the ethics of their profession, which require acting in the best interests of their patients.
Most medical exceptions in abortion bans only allow the procedure to “save the life of the mother.” But there is a wide spectrum of health risks patients can face during pregnancy, and even those that are potentially fatal could fall outside of the exceptions, depending on how the law is interpreted and enforced. Without clarification from legislators and prosecutors on how to handle the real-life nuances that have emerged in hospitals across America, doctors in abortion ban states say they are unable to provide care to high-risk pregnant patients that meets medical standards.
Under threat of prison time and professional ruin, they are finding their personal interests pitted against their patients’ and are overriding their expert training for factors that have nothing to do with medicine, like political perceptions and laws they aren’t qualified to interpret. As a result, some patients are forced to endure significant risks or must travel out of state if they want to end a pregnancy. Sometimes, their doctors aren’t even giving them adequate information about the dangers they face.
Osmundson and 30 other doctors across nine states in which abortion is banned or restricted described to ProPublica the impossible landscape they must navigate in the nearly two years since the Supreme Court struck down Roe v. Wade.
It is one in which fetuses — some with no chance of survival — are being prioritized over their at-risk mothers and oncologists are hesitating to give chemotherapy to cancer patients for fear of legal consequences if it disrupts the pregnancies.
Doctors described the position they’ve been put in — denying abortions to high-risk patients who are begging for them — as “distressing,” “untenable” and “insane.” Speaking out about the broken system felt like the only way to not be complicit, Osmundson said. “It’s going to take physicians coming together and saying: ‘We’re not going to participate in this. We’re going to do what we think is right for patients.’”
Osmundson, who has worked at Vanderbilt for the past eight years, decided to share with ProPublica the inner workings of the hospital’s abortion committee to give the public a rare glimpse into the tortured decisions she and her colleagues are being forced to make. It shows how maternal health care could be dramatically altered across America if Republicans gain control of Congress this fall and succeed in passing the nationwide ban that influential anti-abortion activists have long sought.
In a series of interviews, Osmundson detailed the deliberations in a wide variety of cases and described conversations and emails among doctors. She did not disclose the identities of patients or their individual files. ProPublica was able to confirm details with one patient and three colleagues familiar with the committee, some of whom were not willing to speak publicly for fear of professional repercussions. Vanderbilt declined to comment.
What she shared shows how the strictly written bans fail to account for a broad range of dangerous maternal health risks, leaving doctors to deny abortion requests for medical reasons like warning signs of preeclampsia, a potentially fatal blood pressure condition; complications related to Type 1 diabetes, which can cause vision loss, kidney disease and death; and conditions requiring patients to have their uteruses “cracked open” in order to give birth.
She’s come to believe it’s time to take abortion decisions out of doctors’ hands and shift the final say to hospital lawyers and administrators. In her view, that’s the only way to protect the independent judgment of the medical experts, who could make strong arguments in their patients’ interests using research and data.
“I understand pragmatism,” Osmundson told ProPublica. “I also don’t want to have a patient die and be responsible for it.”
She also thinks hospitals should require doctors to obtain informed consent from patients facing dangerous pregnancy complications, so that providers can’t make decisions on their behalf without counseling them about their risk and getting their response. “In this climate, we’ve really diminished women’s autonomy,” she said. “If a patient says, ‘I don’t want to take on that risk,’ we need to honor that.”
A few months ago, she was on call caring for a patient who had developed severe high blood pressure near 24 weeks, a warning sign for preeclampsia, which can rapidly deteriorate and lead to organ damage or death. With her pregnancy at the edge of viability, the patient requested to have a cesarean section, Osmundson said, even though there was a significant chance the baby might not survive.
Osmundson said she scheduled the surgery. This was not considered an abortion, because the intent was still to deliver a live baby. But after her shift ended, Osmundson recalled, a colleague overrode her and kept the patient pregnant.
Osmundson and her colleagues launched the committee in fall 2022 to address a crisis they were seeing unfold in abortion ban states across the country and at Vanderbilt: Patients facing severe and urgent pregnancy complications were being denied care by hospitals where doctors were terrified about the new legal personal and professional risks.
With strength in numbers, the committee members would back one another up and aim to serve the most patients possible while staying within the law.
Since then, the committee has helped Vanderbilt doctors respond to the most severe emergencies. Abortion requests can hit the committee’s inbox at any hour — at least two a month, but sometimes four in a week. When complications are urgently life-threatening — cardiac failure, Stage 3 kidney disease — doctors often coordinate through a few text messages and sign off that an abortion is medically indicated.
The committee has also developed critical protocols. If a patient’s water breaks before a fetus is viable, the administration considers it a medical emergency because the patient has a high chance of developing sepsis, which can lead to death. In those cases, it’s a blanket policy that doctors can offer abortion care, Osmundson said.
Other cases fall outside of the committee’s power. Osmundson said she has seen some doctors avoid the issue entirely, never informing their patients about the option to terminate their risky pregnancies; those cases never make it to the committee’s attention. The law also makes no exception for sexual assault or fetal anomaly cases, even when the pregnancy is not viable. Doctors direct these and other patients who want abortions to leave the state, if they can. In 2023, Osmundson counted 27 cases of nonviable pregnancies that were referred out of state.
It is those cases in the middle — potentially perilous, but not urgently deadly — that can feel like bombs hitting their inboxes, blasting shrapnel into the rest of their days as they turn over the particulars and try to come to a consensus.
The six doctors, five of whom are women, sometimes call one another up to hash it out. Other times, the discussion unfolds over email and can involve specialists from other departments. They respect one another and know they share the same goals, but the conversations can be heated and emotionally draining.
Last October, a challenging case came before the abortion committee, showcasing the murky limits of Tennessee’s exception.
The patient was seven weeks pregnant and stable, but with a medical history that would make delivery very high risk. Surgeons would need to make a vertical incision on her abdomen — a procedure Osmundson described as “fileting” the uterus — that could lead to permanent bladder or bowel damage due to the patient’s existing complications.
When Osmundson read the file, her mind ticked through worst-case scenarios if things didn’t go well: The patient might need to use an ostomy bag attached to her abdomen to dispel waste. She could suffer severe blood loss or develop sepsis. She could die. The patient already had children and, in a letter to her doctors, requested an abortion.
The challenge for the doctors: The patient had no immediate complications; the potential emergency would not occur until the baby was at full term and doctors were performing surgery. Was it enough to predict that a patient might suffer “substantial and irreversible impairment” or death, based on past case studies? Or did the emergency need to have actually begun?
The law doesn’t say. Nor does it give guidance on how doctors should interpret the spectrum of risk. Was a 50% chance of death or “substantial and irreversible impairment” enough to meet the standard of the law? Twenty percent? Ten? The law says only that an abortion must be “necessary” in a doctor’s “reasonable” medical judgment.
Committee members could see how a zealous prosecutor might challenge that judgment. Doctors like Osmundson often help manage risk for patients who choose to go forward with dangerous pregnancies; some make it through with few long-term issues. It wasn’t hard to imagine a scenario in which a prosecutor held up cases of women who had survived similar complications and pointed to one patient’s abortion as a crime. The penalties for violating the ban include up to 10 years in prison and a $15,000 fine. Doctors can also lose their medical licenses if they are criminally charged. Many have expressed that they would not trust jurors without medical training to evaluate their cases and decide their fate.
In that October case, one doctor argued that the patient’s condition did not fit the definition of a medical emergency because continuing the pregnancy itself would not cause direct harm to an organ — all of the risk would emerge at the time of delivery.
“Who are we to say what is too much or not enough risk?” another wrote. “Where is the line and why do we have to decide that?” But the doctor pointed out that if they offered the abortion, “nurses and other staff will be upset.”
A third wrote: “I unfortunately don’t think this meets the criteria for the law and my interpretation even though it is the ethical right thing to do.”
A fourth: “If one of our purposes is to protect the physicians involved in the care of these patients, I think this case is too risky.”
Osmundson bit her lips as she read the responses. After work, as she cooked dinner for her family and played with her kids, she couldn’t stop thinking about the patient. It was one thing to choose to continue a high-risk pregnancy — another to be forced to. As a doctor who spent her career working with the most difficult cases, she knew better than anyone that even healthy pregnancies could suddenly turn life-threatening.
“I just watched a woman die from liver failure this weekend after a normal uncomplicated pregnancy,” Osmundson told them. “I’m finding it morally repugnant to force anyone to continue a pregnancy for a potential life when the pregnancy poses a real threat to her life.”
If the patient the committee was considering died, Osmundson felt they would all have blood on their hands.
“I cannot deny abortion care to a patient concerned about their medical safety,” she wrote.
The group punted the decision until the university’s ethics committee could weigh in.
The patient was left waiting on a faceless abortion committee to deliver its verdict as the clock ticked.
Soon after, Osmundson learned, the woman was no longer pregnant. Perhaps it was a miscarriage. Or perhaps, Osmundson thought, she had gotten fed up and taken measures into her own hands.
It saved the committee from making a difficult decision. This time.
The predicament is far worse at many other hospitals.
Plenty of doctors ProPublica interviewed don’t work at a well-resourced institution or have an administration that has promised criminal defense if they are prosecuted. And some hospitals rely on state funding, leaving them subject to the demands of lawmakers who could request their emails and protocols, which are public record. Many doctors requested anonymity to speak about sensitive internal matters, fearful they could land on the radar of state officials looking to target abortion providers.
There were wide variations in how their hospitals have navigated the post-Roe reality. Some had abortion committees, but many relied on informal networks among colleagues to make decisions. A few had developed protocols like Vanderbilt’s, but others still require signs of infection or bleeding in order to act, even in cases when a patient’s water breaks before viability. “We are trying to push the idea that the harm does not have to be immediate,” said Dr. Nisha Verma, an OB-GYN and abortion provider in Georgia. “But institutions want to protect themselves.”
Doctors recounted nurses saying they weren’t allowed to treat patients who needed urgent abortions to survive. One was bleeding out. Another was septic. “That’s part of our risk,” one doctor said. “You don’t know who you are working with, who will decide you need to run this by the district attorney.”
Doctors felt similar hesitation from their specialist colleagues, some of whom have balked at having to sign off on any abortion-related paperwork. One OB-GYN described trying to get a cardiologist to evaluate a pregnant patient with heart failure. “We got a ‘Look, we know what you guys are doing and we don’t agree with abortion, so we aren’t going to say she can have an abortion,’” the doctor said.
In other cases, specialists have been afraid to treat patients for fear of accidentally causing harm to a fetus. One OB-GYN said an oncologist at their hospital was reluctant to provide cancer treatment for a patient who wanted to continue their pregnancy, in case chemotherapy were to be misconstrued as an abortion.
Some doctors feel that instead of offering backup, their hospitals have siloed all responsibility to a few providers who would take the fall if an abortion case were challenged. “Care was dependent on each case and who saw the patient and what their risk tolerance was and their views about abortion,” said Dr. Jessica Tarleton, an OB-GYN and abortion provider in South Carolina who left her institution due to its handling of the ban. “It was like chaos all the time.”
Doctors have no clarity on whether they could face repercussions for offering abortions for life-threatening health risks that aren’t active emergencies.
Lawmakers and prosecutors don’t want to offer it.
In Tennessee, legislators sided with an anti-abortion group last year to defeat an effort to include clear exceptions for fatal fetal anomalies and broader health risks. A lobbyist for the group opposed language that would allow doctors to provide abortions to “prevent” emergencies because, he said, “that would mean that the emergency hasn’t even occurred yet.” And Attorney General Jonathan Skrmetti is fighting a legal effort aimed at getting a judge to clarify the ban’s exception; he argues that the state can’t be held liable for doctors “overcomplying” for fear of violating the law. The case is ongoing.
Anti-abortion groups that support the bans have advocated for the narrowest possible interpretation of exceptions. “We would want a stricter standard,” Blaine Conzatti, the president of Idaho Family Policy Center, told ProPublica in November. “The only appropriate reason for abortion would be treating the mother and the unintended consequence is the death of the preborn child.”
Meanwhile, officials have doubled down on their warnings about the consequences if doctors go too far.
Texas Attorney General Ken Paxton fought back against the Biden administration’s federal guidance to offer abortion care for patients with medical complications and threatened doctors with prosecution if they complied with a court’s order to offer emergency abortion care. And in Indiana, the Attorney General Todd Rokita investigated a doctor for sharing with the media that a 10-year-old rape victim had to go out of state to get an abortion.
“There aren’t many people who want to risk or just rely on the goodwill of the legislature and the attorney general or any politician in our state,” one doctor said. Penalties vary by state — in Texas a doctor could face 99 years behind bars.
No doctor has been prosecuted under their state’s abortion ban. But the few public glimpses into judges’ thinking hasn’t provided reassurance. Recently, a Texas court denied a doctor’s request to serve a woman who wanted an abortion because her fetus had a fatal anomaly. The doctor argued the woman shouldn’t be subject to the risks of carrying to term a baby that would not survive. The court said the doctor hadn’t proved her life was in danger.
Will a judge decide the same if a doctor is charged with a felony? Would a jury, or an appellate court, or ultimately the Supreme Court? “The bottom line,” said Dr. Emily Patel, a maternal-fetal medicine specialist in Nebraska, “we don’t know what [the exception] means and won’t know until it’s tested in a court of law.”
No doctor wants to be the first to stand trial. “I don’t know how you can overinterpret the law when you are looking at jail time,” said Dr. Dawn Bingham, an OB-GYN in South Carolina. “A prudent person would hear that and go, ‘Well I guess I will interpret that to be as safe as possible.’”
A year ago, Osmundson said, she could never have imagined arguing to strip her committee of its decision-making power and turning it into an advisory board. But now she believes it’s the only way to shield doctors from the ethical conflict of denying patients evidence-based care. “I feel like these committees are kind of making physicians become complicit in an unethical and unjust system,” she said.
Dr. Mack Goldberg, her committee colleague, knows the position perhaps better than anyone else. Unlike most of his colleagues, including Osmundson, he actually performs abortions; since clinics shuttered in the wake of the ban, he’s one of the only people in the state with the expertise and institutional support to do so for medical complications.
He knows the hospital submits paperwork to the state after each one. And while he recognizes that his colleagues are putting their names on the decisions, he feels more exposed. He often can’t shake the feeling of being constantly on call, his livelihood perpetually on the line, a burning question in the back of his mind: “When push comes to shove, if I ever got trudged through a court case, how many people will truly have my back?”
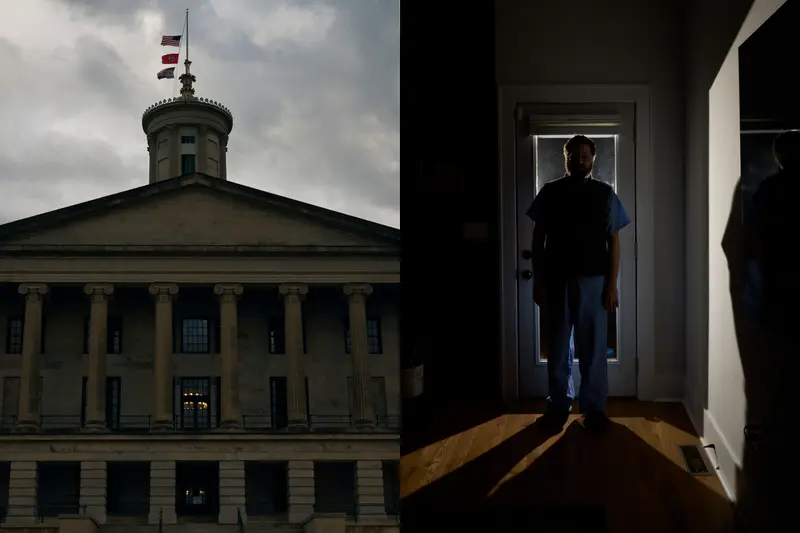
Credit:
Stacy Kranitz, special to ProPublica
Despite all of the anguish it causes him to turn away some patients, Goldberg disagrees with Osmundson. He believes it’s important for doctors to continue walking the tightrope: Do as much as possible with the support of colleagues and their institution, while being honest with patients about their risks and options. He feels the committee has made it possible for him to save some lives by acting quickly, and he doesn’t want to leave the call to hospital administrators and lawyers, who may be even more risk averse.
”We are on the front lines,” he said. “At the end of the day, the patients are staring right in our faces.”
Late last year, he sighed heavily as he counseled the woman whose baby was developing without a skull and gently told her what he tells all of his patients in her position: that he had the training to help her, but because of Tennessee’s laws, he might face prosecution and jail time if he did. He had a baby at home and couldn’t take that risk, he explained. Instead he would refer her to options outside the state.
The patient, Charlotte Miller, told ProPublica she understood and appreciated his thorough counseling. But she was stricken to realize it would have been different had they been in her home state of Colorado.
When the 22-year-old sat across from Goldberg in his office, all she knew was that she didn’t want to spend the next six months putting her body through the hardships of pregnancy to give birth to a baby that would never survive.
Her first pregnancy had been challenging. She struggled with worsened asthma and endometriosis, a painful condition in which tissue grows outside of the uterus. The toll on her mental health alone would be enormous, she believed, and she didn’t want to risk any unexpected complications that could make getting pregnant again more difficult. She desperately desired another child, but in this case, the best option, she was certain, would be to deliver her baby as soon as possible — to have the chance to hold him and say goodbye.
Instead, her family would have to scrape together more than $1,200, a week of her partner’s paycheck as a waiter, so she could travel to a clinic in Illinois. There, her only choice would be a dilation and evacuation procedure while unconscious, not a delivery in which her baby could emerge intact and she could hold him in his last moments. Before it came to that, she lost the pregnancy naturally.
She’d been unaware of the committee’s debate about her health risks. When she learned of it, it only affirmed what she’d come to believe: “It’s just so disheartening to me that doctors can want to provide me care and not be able to because of what a law says, for fear that they would have repercussions.”

