On New Year’s Day 2020, I was zipping up my fleece to head outside when the phone in the kitchen rang. I picked it up to find a reporter on the line. “Dr. Fauci,” he said, “there’s something strange going on in Central China. I’m hearing that a bunch of people have some kind of pneumonia. I’m wondering, have you heard anything?” I thought he was probably referring to influenza, or maybe a return of SARS, which in 2002 and 2003 had infected about 8,000 people and killed more than 750. SARS had been bad, particularly in Hong Kong, but it could have been much, much worse.
A reporter calling me at home on a holiday about a possible disease outbreak was concerning, but not that unusual. The press sometimes had better, or at least faster, ground-level sources than I did as director of the National Institute of Allergy and Infectious Diseases, and reporters were often the first to pick up on a new disease or situation. I told the reporter that I hadn’t heard anything, but that we would monitor the situation.
Monitoring, however, was not easy. For one thing, we had a hard time finding out what was really going on in China because doctors and scientists there appeared to be afraid to speak openly, for fear of retribution by the Chinese government.
In the first few days of 2020, the word coming out of Wuhan—a city of more than 11 million—suggested that the virus did not spread easily from human to human. Bob Redfield, the director of the Centers for Disease Control and Prevention, was already in contact with George Gao, his counterpart in China. During an early-January phone call, Bob reported that Gao had assured him that the situation was under control. A subsequent phone call was very different. Gao was clearly upset, Bob said, and told him that it was bad—much, much worse than people imagined.
“We don’t know what’s going on with this virus coming out of China right now,” I told the group assembled in a conference room at the National Institutes of Health. This was January 3, just 48 hours after the reporter had called me at home. The scientists sitting around the table, led by Vaccine Research Center Director John Mascola, knew what I was going to say next: “We are going to need a vaccine for whatever this new virus turns out to be.”
Among those present was Barney Graham, a gentle giant of a man at 6 feet 5 inches tall, and one of the world’s foremost vaccinologists. For years, Barney had been leading a group of scientists trying to develop the optimal immunogens for vaccines injected into the body. (An immunogen refers to the crucial part of any vaccine that generates the immune response.) They had been working with Moderna on a vaccine platform called mRNA, the result of groundbreaking research conducted over many years by Katalin Karikó and Drew Weissman, who would win the Nobel Prize in 2023. “Get me the viral genomic sequence,” Barney said, “and we’ll get working on a vaccine in days.”
At this point, an FDA-approved vaccine had never before been made using mRNA technology, and although a lot of skepticism remained, my colleagues and I were very optimistic about it. Compared with other vaccines, the mRNA process is faster and more precise. The team needed the coronavirus’s genomic sequence so that it could pick out the part that codes for the spike protein (the immunogen) and, together with Moderna, use it to make the correct mRNA.
Only a week later, on January 10, I received an excited phone call from Barney: Scientists had just uploaded the SARS-CoV-2 sequence to a public database. Barney then immediately contacted a company that produces artificial strings of genetic code. He placed an order for the nucleotide sequence, and this lifesaving product was delivered in a small test tube packaged in a FedEx envelope. The modest charge was put on a credit card.
But soon after, Barney made a sobering point: A full-blown vaccine effort, including clinical trials, was going to cost a lot of money, far beyond what was in the Vaccine Research Center’s budget. I told him not to worry. “If this thing really explodes, I promise you, I will get us more money. You just go and make your vaccine.”
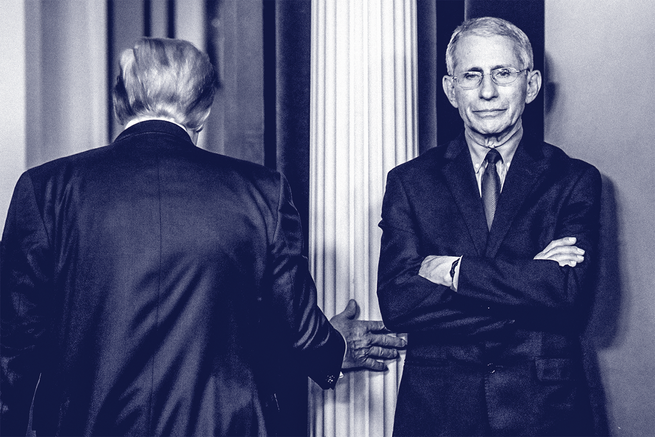
About an hour into a meeting in the White House Situation Room on January 29, concerning how to evacuate U.S. citizens from Wuhan, President Donald Trump walked in. The first thing he did, to my great surprise, was look right at me.

January 29. (Joyce N. Boghosian / White House)
“Anthony,” he said, “you are really a famous guy. My good friend Lou Dobbs told me that you are one of the smartest, knowledgeable, and outstanding persons he knows.” I gulped. Thus began my first extended conversation with the 45th president of the United States. A big, imposing man, Trump had a New York swagger that I instantly recognized—a self-confident, backslapping charisma that reminded me of my own days in New York. For the next 20 minutes, as we discussed the new virus, the president directed many of his questions my way. I had met Trump only once before. In September 2019, I had been part of a group invited to the Oval Office for the signing of an executive order to manufacture and distribute flu vaccines. Prior to that, I had sometimes wondered what it would be like to interact with him. He had shocked me on day one of his presidency with his disregard of facts, such as the size of the crowd at his inauguration. His apocalyptic inaugural address also had taken me aback, as had his aggressive disrespect for the press. But at that brief signing ceremony, I had found him far more personable than I’d expected. Of course, I had no idea in January 2020 what the months and years ahead would be like.
I had confronted other terrible outbreaks over the course of my career—HIV in the 1980s, SARS in 2002 and 2003, Ebola in 2014, Zika in 2015—but none of them prepared me for the environment I would find myself in during the coronavirus pandemic. The nation was and is extremely polarized, with a large portion of Americans reflexively distrustful of expertise. On social media, anyone can pretend to be an expert, and malicious information is easily amplified. Soon I would come to learn just how dangerous these conditions can be.
A code red went off in my mind during the week of January 23, when I saw photos in a newspaper showing that the Chinese government was quickly erecting a 1,000-bed prefabricated hospital. At that point, the virus had reportedly killed just 25 people and infected about 800, according to data the Chinese had released. Time out, I thought. Why would you need that many hospital beds when fewer than 1,000 people are infected? That was the moment I suspected we could be facing an unprecedented challenge, and my anxiety took a sharp turn upward.

By the very end of January, we were hearing that the cases in China were increasing by about 25 percent a day. Reportedly, more than 9,000 people were infected, and 213 people were dead. The number of infections in a single month had surpassed the 2002–03 SARS outbreak. The United States had discovered its first known case of this novel coronavirus on January 20; a 35-year-old man had returned home to Washington State from Wuhan with a severe cough and a fever. The CDC had already begun screening passengers at several U.S. airports, taking their temperature and asking them about symptoms such as a sore throat and a cough. We began to wonder: Should we recommend closing the United States to travelers from China? On January 31, seated in front of the Resolute desk, Health and Human Services Secretary Alex Azar, the CDC’s Bob Redfield, and I explained the details of a proposed travel ban to the president. He posed several questions specifically to me about whether I was fully on board with the ban. “It is an imperfect process with some downsides, Mr. President, but I believe it’s the best choice we have right now,” I told him. Later that day, the Trump administration announced that travel restrictions would go into effect.
The White House communications team began arranging for me to appear on news shows. The entire world was transfixed by this rapidly evolving outbreak, and I became the public face of the country’s battle with the disease. This was useful, in that I could both try to calm the country’s anxieties and provide factual information. But it also led to the gross misperception, which grew exponentially over time, that I was in charge of most or even all of the federal government’s response to the coronavirus. This would eventually make me the target of many people’s frustration and anger.
On February 11, the World Health Organization officially designated the disease caused by the novel coronavirus as COVID-19, which was now spreading relentlessly around the world. And in the midst of this, the CDC, the country’s premier public-health agency, was stumbling badly.
The agency traditionally had a go-it-alone attitude, excluding input from outside sources. Its personnel were talented and deeply committed professionals. I respected them, and many were friends. But the CDC’s approach, which is based on tracking symptoms, was poorly suited to dealing with a swiftly spreading disease in which, it would later turn out, more than a substantial portion of the transmissions come from people who are asymptomatic. The CDC was slow to recognize and act on that.
Another vulnerability was the way the CDC was set up to collect data. Rather than obtaining data firsthand, the agency depended on public-health departments around the country—but those departments did not consistently provide complete, up-to-date data. Some provided information reflecting what had occurred weeks earlier, not the day before. As the disease kept spreading, what was actually happening was always far worse than what the CDC’s data were telling us at the time. Public-health officials had to constantly play catch-up.
The CDC had an outstanding track record for quickly creating tests for diseases like Zika. With COVID, however, instead of immediately partnering with the diagnostic industry, it started from scratch with a test that turned out to be defective. The agency then failed to fix the defect, and wasted even more time in developing adequate testing. February was a lost month as a result.
Although the CDC struggled, there was no mistaking the message delivered on February 25 by its director of immunization and respiratory diseases, Nancy Messonnier. She told reporters that a pandemic in the United States was no longer a matter of if but when, and that we should prepare to close schools and work remotely. “Disruption to everyday life may be severe,” she announced. Nancy did the right thing: She told Americans the truth. But not surprisingly, her statement caused a firestorm. The media erupted, and the stock market plummeted nearly 1,000 points. Trump was furious.
The next day, he announced that Vice President Mike Pence would take over for Alex Azar as the head of the White House coronavirus task force. I met Pence the day he ran his first task-force meeting. He was soft-spoken and always solicited the medical opinions of the physicians on the task force. He listened carefully to our answers, often asking astute follow-up questions and never pretending to understand something if he did not. But I also picked up on little things that indicated how differently this administration operated from previous ones. Vice presidents are always publicly loyal to the president; that is part of the job. But Pence sometimes overdid it. During task-force meetings, he often said some version of “There are a lot of smart people around here, but we all know that the smartest person in the building is upstairs.”

Others joined Pence in heaping praise on Trump. When the task force held teleconferences with governors, most of the Republicans started by saying, “Tell the president what a great job he is doing.” But a couple of days after Nancy’s bombshell announcement, when I got a surprise phone call from Trump at 10:35 p.m., I did not flatter him. What I did do during our 20-minute conversation was lay out the facts. I encouraged him not to underplay the seriousness of the situation. “That almost always comes back to bite you, Mr. President,” I said. “If you are totally honest about what is happening with COVID, the country will respect you for it.” He was courteous to me, and as we hung up, I felt satisfied that he had heard what I’d said.
I was worried about community spread, and I was particularly focused on Seattle. A longtime colleague called me from the city on March 3 and told me that 380 people with flu-like symptoms had been screened in four emergency rooms. Four had tested positive for COVID, a roughly 1 percent infection rate—that may not sound like much, but it was a clear signal that the virus was spreading among those unaware that they had been exposed. That meant the 1 percent was only a tiny fraction of what was actually already happening. When I brought this information to the task-force meeting, neither Pence nor Treasury Secretary Steven Mnuchin seemed to fully appreciate the seriousness of what I was telling them. While I was warning them of the impending disaster, the president was declaring outright to the press that the situation was under control. Without deliberately contradicting him, I kept repeating that things would get worse, and indeed they did.
Then, in one Oval Office meeting, I mentioned to Trump that we were in the early stages of developing a COVID vaccine. This got his attention, and he quickly arranged a trip to the NIH. During his visit, Barney Graham told the president that within a couple of weeks, a Phase 1 trial would likely begin. The president asked, “Why can’t we just use the flu vaccine for this virus?” It was not the first or the last time that he seemed to conflate COVID with influenza.
People associate science with immutable absolutes, when in fact science is a process that continually uncovers new information. As new information is uncovered, the process of science allows for self-correction. The biological and health sciences are different from the physical sciences and mathematics. With mathematics, two plus two equals four today, and two plus two will equal four 1,000 years from now. Not so with the biological sciences, where what we know evolves and uncertainty is common.
On March 8, I appeared on a 60 Minutes broadcast in a segment about COVID. At one point, I told the interviewer, “Right now in the United States, people should not be walking around with masks.” I was expressing not just a personal opinion, but the consensus at the time—a view shared by the surgeon general and the CDC.
The supply of masks was already low. One fear was that there would be a stampede, and we would create an even greater shortage of masks needed by the health-care workers taking care of very ill COVID patients. Although there was accumulating evidence that the virus was spread by aerosol, this was not widely accepted, certainly not by the WHO. When additional information became available—including that the virus was readily spread by infected people who had no symptoms—we advised the public to wear masks. But this was how I became the public-health official who, very early in the pandemic, instructed people not to wear a mask. Later, my words would be twisted by extreme elements in an attempt to show that I and other scientists had misled the public, that we could not be trusted, and that we were flip-floppers.
What I came to realize is that our country is more profoundly divided than I’d ever understood. I remember a time when people expected diverse political opinions. You didn’t have to agree, but you respected one another enough to listen. Now the partisanship is so intense that people refuse to even try. They ignore facts in favor of tribal politics. That’s how you wind up with dangerous conspiracy theories. The controversy over masks illustrates a fundamental misperception of how science works. In reality, our understanding of COVID continually evolved, and our medical advice had to change to reflect this.
March 2020 was when COVID became frighteningly real to Americans. This was also around the time I started waking up with a jolt at 4 a.m. to stare at the ceiling with worry. I believe Trump thought that COVID would be temporary: A little time goes by, the outbreak is over, everyone goes back to work, and the election cycle can begin. He could not have imagined that the pandemic would go on for such a long time. I think this explains why he repeatedly asked me and others whether COVID resembled the flu. He desperately wanted the pandemic to disappear, just as flu does at the end of the flu season. Tragically, COVID was not the flu, and it did not vanish. Just the opposite. And so, with the ghastly reality setting in, Trump began to grab for an elixir that would cure this disease. Along came hydroxychloroquine.
Trump began hearing from the Fox News star Laura Ingraham and others who were promoting the drug as a COVID treatment. People have long taken hydroxychloroquine to prevent or treat malaria. It is also used to treat inflammatory and autoimmune diseases such as lupus and rheumatoid arthritis. Soon Trump began touting it to millions of worried Americans at our now-daily press briefings. But there were no clinical studies proving that this antimalarial drug would alleviate COVID. And it might even hurt people. The president seemed unable to grasp that anecdotes of how hydroxychloroquine might have helped some people with COVID did not translate into solid medical advice. This is when I realized that eventually, I would have to refute him publicly. This was not the White House I had known, and I’d been advising presidents since the Reagan administration. The differences were going to dramatically affect the way I could do my job. “Hydroxychloroquine doesn’t work,” I told reporters. After that, they would inevitably ask me if I agreed with something Trump had said, such as the idea that COVID would disappear “like a miracle.” I would then have to respond with the truth: “Well, that’s not going to happen.”
I took no pleasure in contradicting the president of the United States. I have always had a great deal of respect for the Office of the President, and to publicly disagree with the president was unnerving at best and painful at worst. But it needed to be done. I take very seriously a statement in the first chapter of Harrison’s Principles of Internal Medicine, of which I have been an editor for 40 years: “The patient is no mere collection of symptoms, signs, disordered functions, damaged organs, and disturbed emotions. [The patient] is human, fearful, and hopeful, seeking relief, help, and reassurance.” This compels me to always be honest; to be unafraid of saying that I do not know something; to never overpromise; to be comforting, yet realistic. Admitting uncertainty is not fashionable in politics these days, but it is essential in my work. That’s the beauty of science. You make a factual observation. If the facts change, the scientific process self-corrects. You gather new information and data that sometimes require you to change your opinion. This is how we better care for people over time. But too few people understand the self-corrective nature of science. In our daily press conferences, I tried to act as if the American public were my patient, and the principles that guided me through my medical career applied.
There is a widely circulated photo of me from a White House press briefing on March 20, in which I put my hand to my forehead in response to a comment the president had made. That day, Trump was especially flippant. He was standing with Secretary of State Mike Pompeo, making one provocative statement after another. Then he said, “Secretary of State Pompeo is extremely busy, so if you have any questions for him right now could you do that because … I’d like him to go back to the State Department or, as they call it, the ‘Deep State’ Department.” I had a moment of despair mixed with amusement. I put my hand to my forehead to hide my expression. This is when things began to get difficult for my family and me.
In late March, officials monitoring the dark web started to see a considerable amount of hostility and threats directed toward me. The problem was that a hard-core group saw me as a naysaying bureaucrat who was deliberately, even maliciously, undermining Trump. They loved and supported the president and regarded me as the enemy. To them, my hand-to-forehead moment validated what they already believed about me.

As a result, I was assigned a security detail. For years, AIDS had made me a target, but that was largely before social media. Back then, I used to get one or two insulting letters a month, mostly homophobic rants, sent to my office at the NIH. Now my family and I were barraged by emails, texts, and phone calls. I was outraged that my wife, Christine, and our daughters were harassed with foul language and sexually explicit messages, and threatened with violence and even death. I was angry and wanted to lash out. But these direct expressions of hatred did not distract or frighten me. I did not have time for fear. I had a job to do.
My training as a physician in a busy New York City hospital had taught me to push through crises and fatigue, to not feel sorry for myself. During the pandemic, Christine also insisted that I balance the demands of work with taking care of myself. (“You are going to bed at a decent hour, you are going to eat regular meals, and you are going to carry a water bottle,” she said in a way that left no room for argument.) Her advice helped me get through everything that followed.
But in the ensuing years, I also came to realize that addressing the root cause of our country’s division is beyond my capabilities as a scientist, physician, and public servant. That doesn’t mean I’ve given up hope that the country can be healed. I believe scientific education is more crucial now than it has ever been in American history. Children should learn what the scientific process is, how it works, and that it self-corrects. Most of all, I believe we need to reclaim civility. To do so, we need to understand that we’re all more alike than we are different—that we share common goals for ourselves and for our communities. We need to learn to talk to one another again. And we need to figure that out before the next pandemic hits.
This article was adapted from Anthony Fauci’s book On Call: A Doctor’s Journey in Public Service. It appears in the July/August 2024 print edition with the headline “The First Three Months.”
When you buy a book using a link on this page, we receive a commission. Thank you for supporting The Atlantic.


