Angel had wanted to talk to a doctor before she took the pills to end her pregnancy, worried about how they might interact with medication she took for her heart condition.
But in her home state of Oklahoma, where almost all abortions are banned, that wasn’t an option.
The pain kicked in after about an hour, around midnight on a Sunday in January, eventually becoming sharp enough that the 23-year-old said she struggled to stand. While Angel would be fine by the next morning, she worried that something might be very wrong as she lay on the cold bathroom tile, her body racked by some of the worst pain she could remember.
When Angel’s fiancé came in to check on her, she was having diarrhea while vomiting into their popcorn bowl.
“F—,” she remembered yelling, over and over. “I feel like I need to push.”
Overwhelming evidence shows that abortion pills are safe and effective, and that many patients who take them go through the process without much difficulty, experiencing little more than the sharp cramping and bleeding of an unusually heavy period. That is true even when the pills, approved by the U.S. Food and Drug Administration with a prescription for use through 10 weeks of pregnancy, are taken somewhat independently — administered by a doctor over text, email, or a call and mailed to the patient at home.
But the experience can feel very different in states where abortion is illegal. As more women in states with abortion bans choose to end their pregnancies on their own, without directly interacting with a medical professional, they are thrust into a largely ad hoc, unregulated system of online and grass-roots abortion pill distributors — an experience that, while deemed generally safe by medical experts, can be confusing, scary and, at times, deeply traumatic.
“I feel like I need to push.”
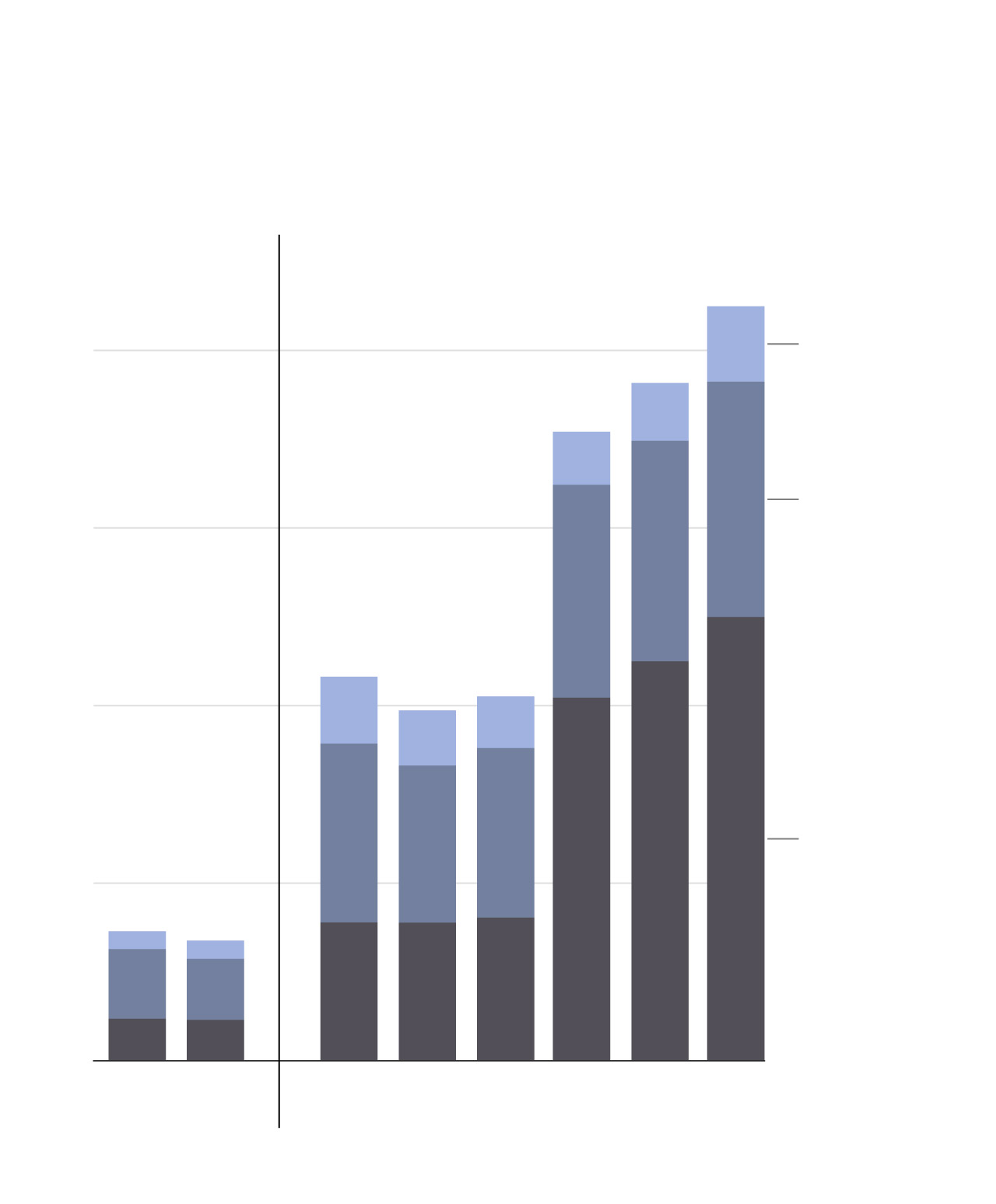
“Self-managed” abortions increased dramatically after Roe v. Wade was overturned — with women in antiabortion states obtaining pills through several distinct channels. At least 6,000 women every month in states with bans are now receiving pills from Aid Access, a Europe-based online clinic that prescribes the medication without requiring a patient to interact with a doctor in real time, according to founder Rebecca Gomperts. Thousands of others are turning to at least 25 nonmedical websites that sell the pills, or one of several volunteer-led networks that distribute them for free.
With abortion clinics shuttered across the South and Midwest, many women said they have nowhere to go to confirm that their abortion pill supplier is “legit” or that their symptoms after taking the medication are normal. They worry that a call to a doctor or a trip to the emergency room could land them in jail. And while abortion rights advocates have tried to build new infrastructure to support women in these situations — with volunteer doctors answering phone calls or former abortion providers staffing the occasional bricks-and-mortar office in an antiabortion state — organizers say that such resources are no replacement for the array of choices women had before Roe fell.
The demand for self-managed abortions in states with bans, already enormous, is sure to increase dramatically in the coming weeks, as strict new abortion laws take effect in Florida and Arizona — the result of two recent court rulings.
“This is not the way health care should be,” said Linda Prine, a New York-based doctor who prescribes pills through Aid Access and co-founded a hotline for people taking them. “All the options have been taken away from people by these bans and this is all that’s left,” she added, referring to the networks providing pills for women self-managing their abortions.
“It really is all we can do.”
Chart of monthly supplies of self-managed abortions Pre- and Post-Dobbs from online vendors, telemedicine and community networks
Adding to the difficulty is a polarized political debate with dueling narratives about what it’s actually like to take abortion pills. Antiabortion activists say the pills are highly dangerous, or even deadly, for pregnant women — false assertions based largely on studies that have now been retracted by the journal that published them. Meanwhile, many abortion rights advocates describe the experience as straightforward and easy to handle on your own, a characterization that some women say glosses over what can be a more complicated reality of ending a pregnancy alone in your bathroom.
The Washington Post spoke with more than three dozen doctors, advocates, leading researchers, and women who took the pills in states where abortion has been banned since Dobbs v. Jackson Women’s Health Organization, the Supreme Court case that overturned Roe in June 2022. Over the phone and in person, many women described experiencing deep anxiety and uncertainty about doing something they assumed was illegal. These feelings often intensified after they took the medication, with some not expecting the level of pain or amount of bleeding they would experience, or how much of the fetus they would see. A few used the pills later in pregnancy than the FDA recommends.
“I wish I would have known that it wasn’t just blood clots. … I was really confused and shocked,” said Briana, a 34-year-old in Alabama who took pills she ordered online when she was at least five weeks beyond the FDA’s 10-week limit. Like other women interviewed for this article, Briana spoke on the condition that her last name not be used so she could discuss sensitive medical information in a state that outlaws abortion — describing her experience in graphic detail because she said she wanted other women to know what to expect.
The complex legal landscape can be hard to understand. Abortion bans do not allow people seeking abortions to be prosecuted, targeting only doctors and others involved in facilitating the abortion. But people have been charged under other laws for self-managing their abortions, especially later in pregnancy.
A legal challenge to the abortion drug mifepristone brought by conservative advocates — which drew skeptical questions from the Supreme Court during oral arguments last month — seeks to further restrict the post-Roe landscape by requiring in-person medical visits for all legally administered medication abortions. Such a change could prevent U.S.-based medical providers from mailing pills into antiabortion states under “shield laws,” recently enacted in a handful of blue states, that protect doctors from prosecution under red state bans.


In Oklahoma, Angel ordered her pills from Aid Access, according to emails reviewed by The Post, and took them five to six weeks into her pregnancy. She’d told doctors at the online clinic about her heart medication when she filled out its online form, she said, but no one ever reached out about it — a silence easily explained, Prine said, because Angel’s medication is not one that would raise concerns.
Angel had no way of knowing that.
Sitting on the toilet, she could hear her heart pounding in her ears. She placed two fingers on the side of her neck to take her pulse and started a timer, she recalled — counting about 190 beats per minute.
With her heart condition, she said, she was supposed to seek medical attention if her heart rate got that high.
Angel had no idea who to call. She vaguely remembered a hotline number in the Aid Access instructions, but figured the line would be closed that time of night. The hospital didn’t feel like an option, either: She worried about the questions she might get from suspicious doctors if she showed up at the emergency room.
She closed her eyes and tried to steady her breath, determined to keep her heart rate down. Then she spoke to herself as she imagined a doctor might.
“You will be okay,” said Angel, who would wake up the next morning no longer pregnant, the worst moments of her abortion behind her.
“This pain can’t last forever.”
“Your body will be just fine.”
“Your uterus knows what to do.”
A doctor answers panicked calls
“It’s normal to be scared.”
“Just wait it out.”
“Call back any time.”
Linda Prine was answering a few emails, coffee mug in hand, when her cellphone rang.
“Hi, this is the hotline doctor,” the 72-year-old said from her New York City home one Sunday morning in January. “Can I help you?”
The voice Prine heard was quiet and scared — belonging to a 15-year-old with an area code in a state with an abortion ban who had taken pills and passed a fetus larger than she’d expected.
Unable to flush the fetus down the toilet, the girl asked about throwing it away.
She was young enough to be Prine’s granddaughter.
Prine cradled the phone in both hands and leaned in, trying to channel every ounce of reassurance and understanding she could muster through the phone line.
“There’s nothing in there that’s traceable back to you,” she said. “As long as you don’t tell anybody.”
The girl asked if the abortion made her a bad person.
“No it doesn’t,” Prine said. “Not a bit.”
“You are doing what’s right for you and your future family,” she added, her voice firm.
“This way you can be a good mom when you’re ready to be a good mom.”

A semiretired family medicine physician, Prine co-founded the Miscarriage and Abortion Hotline in 2019 as a resource for people self-managing miscarriages or abortions at home. She got the idea from Gomperts, of Aid Access, who had already been mailing pills to Americans who struggled to access abortion. The American patients had a lot of questions and concerns about ordering pills outside a formal health-care setting, Gomperts told Prine — and her inbox was constantly flooded with emails.
They needed a U.S.-based doctor to call.
“You are doing what’s right for you and your future family.”
Calls to the hotline surged after Texas enacted an early law banning most abortions in the fall of 2021, Prine said, and again after new abortion bans took effect across the South and Midwest when Roe fell. Now the line is staffed by over 50 U.S.-based medical providers who volunteer their time, a mix of doctors, midwives, nurse practitioners and physician assistants with experience in abortion care. The doctors who run the hotline recruit volunteers through word-of-mouth recommendations, then administer a few hours of virtual training before they start.
In interviews, Prine stressed that hotline doctors are not practicing medicine under their licenses or establishing a doctor-patient relationship — a posture Prine said legally protects the physicians. By design, the hotline volunteers don’t ask for the names, locations or full medical histories of the people who call. On the hotline’s website, a disclaimer notes that they are not offering “legal or medical advice,” and that the information they provide “does not substitute for the … advice of a doctor.”
The hotline typically receives roughly 30 calls and 50 texts from people every day. Many say they are in states that ban abortion.
“They’ll say, ‘I’m in a state where this is illegal, so I can’t go get medical care. I want to check in and make sure everything is going okay,’” Prine said.
She and her colleagues hear the same questions again and again: Am I bleeding too much? Am I not bleeding enough? Is it normal to have this much pain? People call to see if they can drink alcohol or smoke marijuana after taking the pills. One woman asked whether it was safe to walk up the stairs.
[What to know after taking abortion pills]
Anxiety and uncertainty are common even among patients who receive the medication at an abortion clinic in a state where abortion is legal, said Prine — because they’re at home by the time they start feeling the full effects.
“People from anywhere can be freaking out because everyone is taking these pills at home alone,” Prine said.
Still, some feel better taking the pills after having a direct conversation with a medical professional. Since Dobbs, many women in antiabortion states who have the resources to travel have continued to leave the state to obtain pills at a clinic instead of ordering online, preferring the experience of being face to face with a doctor, even if it means a long drive or a flight.


For those who choose to self-manage their abortions, Prine said, she is there to offer reassurance that their experiences are nothing out of the ordinary, and that they almost certainly don’t need to go to the emergency room. A medication abortion is just like a miscarriage, she’ll tell them, with hundreds of women going through the same process every day.
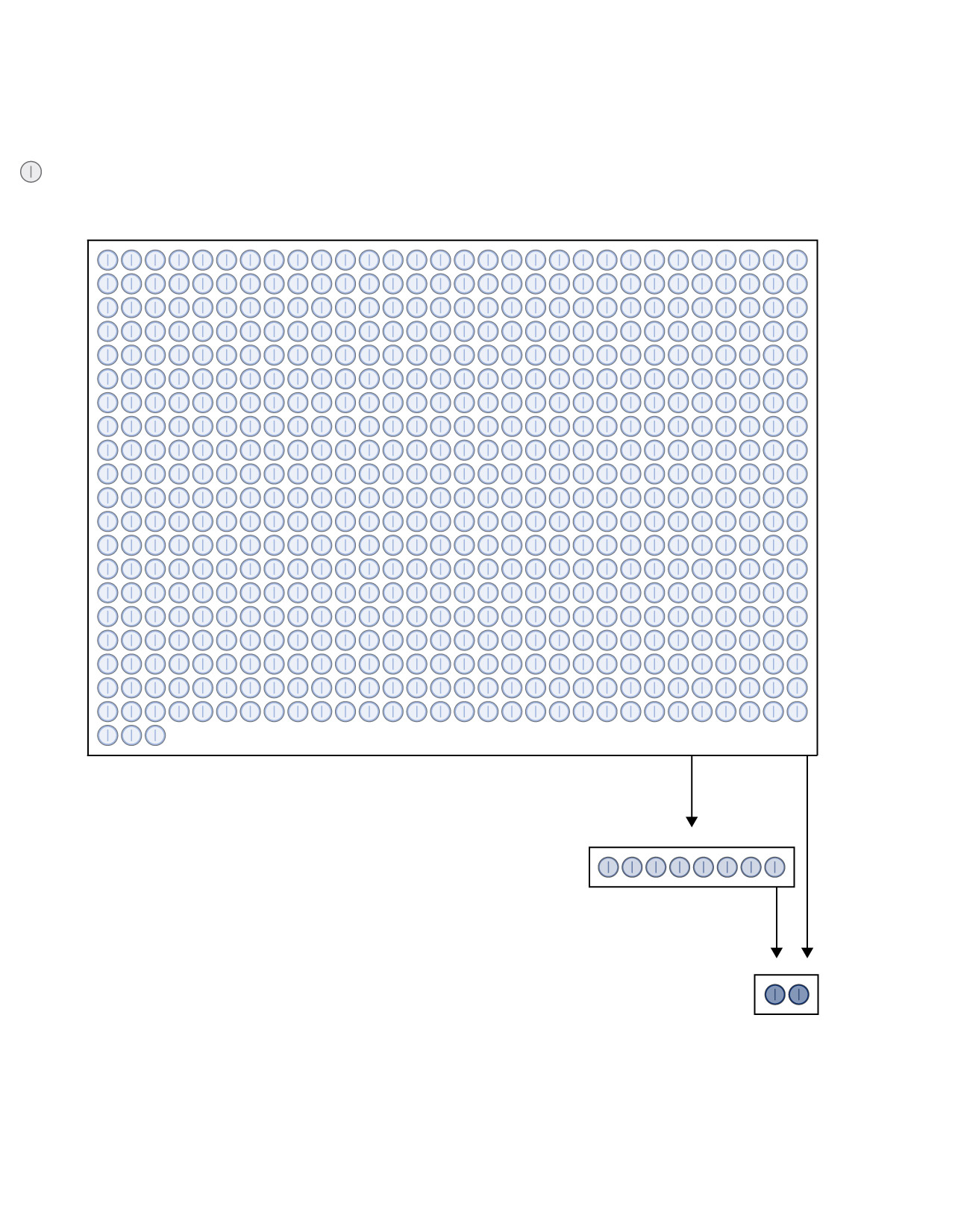
Of the approximately 5.9 million patients in the United States who took mifepristone — the first drug in a two-step medication abortion regimen — between its 2000 approval and December 2022, just 32 died, according to the FDA. Those cases, the agency says, “cannot with certainty be causally attributed to mifepristone.” Major adverse events — in which a blood transfusion, major surgery or overnight hospital stay is required — occur in fewer than 0.5 percent of cases, a figure that remains the same whether a patient has met with a doctor in person.
A significantly larger share of patients who take abortion pills seek emergency care, ranging from 1.3 to 8 percent in leading studies.
Chart showing the number of patients that went to an emergency department, received treatment and experienced a serious adverse event in a recent study.
Antiabortion activists portray those emergency room visits as an indication of a safety issue, but leading medical experts say they instead highlight the confusion and fear that many women experience after taking the pills. Patients often go for a gut check, doctors and medical researchers said, wanting to confirm that they’re not bleeding too much, or that the pills worked and they are no longer pregnant. Studies show that 35 to 50 percent of people who go to an ER after taking abortion pills receive no treatment.
“With medication abortion, there’s no one saying, ‘You’re doing great. This is normal,’” said Ushma Upadhyay, a professor at the University of California at San Francisco and a leading researcher on the safety of abortion pills, drawing a distinction between the pill and a surgical procedure. “Often people are going through it alone, so they want to know everything is okay.”
On the hotline, Prine said she’s felt the need to send someone to the emergency room only once in nearly five years.
“Your uterus knows what to do,” Prine told a woman who called that January morning with reports of unexpectedly heavy bleeding. “It’s going to take care of itself.”
Others in the medical community are quicker to suggest that someone be seen in person.
On the infrequent occasions when a patient calls with concerns about their medication abortion, Clayton Alfonso, an OB/GYN at Duke University, said he’ll try to evaluate how much she is bleeding and how her body is tolerating the blood loss. But he said it can sometimes be difficult to make those assessments over the phone.
“When you take a patient call, it’s always hard because their definition of heavy bleeding could be different from my definition of heavy bleeding,” said Alfonso, adding that he usually tries to bring patients into his clinic if he has space on the schedule. “I would much rather see someone than leave someone in limbo at home not knowing what to do.”
In states with abortion bans, the emergency room is often the only option for women who want in-person care during their medication abortions. Even if they say they had a miscarriage — a condition that presents with symptoms indistinguishable from a medication abortion — many women in these situations have bad experiences at the hospital, Prine said, encountering physicians who provide inaccurate information or ask suspicious questions about why they’re bleeding.
“Your uterus knows what to do.”
Prine said she recognizes that the landscape for self-managed abortions is tenuous. The antiabortion movement is ready to seize on any experience with pills that is difficult or complicated, she said, especially the relatively rare cases in which women take pills later in pregnancy.
At the Conservative Political Action Conference last year, prominent antiabortion activist Abby Johnson said women are delivering “fully formed babies” in their bathrooms — a false description of what women see during a medication abortion, even in the second trimester.
“They’re passing these babies into the toilet,” said Johnson, founder of the antiabortion group And Then There Were None. “Then these women have to make a decision: What do I do with this fully formed baby?… Do I flush my child down the toilet?”
These kinds of incendiary attacks make it hard for abortion rights advocates to discuss the details of a medication abortion later in pregnancy, said Prine and Gomperts — because the specifics could be weaponized by the antiabortion movement.
As a result, Prine said, women who take pills later in pregnancy are sometimes surprised by what they see.
“How much bleeding is normal?”
“Do I push it out?”
A woman struggles to pass her pregnancy
“Should I go to the hospital?”
“I’m totally alone.”
At her home in Alabama, Briana waited to take the pills until she’d put all of her children to sleep.
The cramps in her lower back came first, followed by full-body chills and, eventually, contractions more painful than those she remembered from childbirth.
After lying in bed for two hours, Briana felt something “pop” under the comforter, followed by a gush of warm liquid seeping down her legs. She ran to the bathroom, she recalled in interviews and a journal entry, where she felt a mass larger than her palm drop into the toilet.
“This can’t be happening,” she thought to herself.
Then she looked down to see a bloody umbilical cord dangling between her legs.
When the pills first arrived in the mail a few days earlier, in April 2023, Briana had expected her experience would be more difficult than most. The doctors who administered the medication through Aid Access cautioned Briana that they “do not like to recommend medical abortions” as far into pregnancy as she would be when the pills reached her, according to emails reviewed by The Post.
Briana felt she had no choice. By the time she found out she was pregnant, she was already 11 or 12 weeks along. The abortion clinic she’d called in a different state, more than a six-hour drive from her home in Alabama, where abortion is banned, was booked for surgical procedures for over a month, busy treating patients from other antiabortion states across the South. She spent nearly two weeks researching her other options, then the pills she ordered took two weeks to arrive.
The 34-year-old was struggling to support the kids she already had.
“I didn’t want to take any more away from them … time, attention, money,” said Briana, who estimates that she was 15 or 16 weeks along when she took the pills.
“This can’t be happening.”
Experts and advocates say it is relatively rare for women to self-manage their abortions well beyond the FDA’s 10-week limit, particularly since passage of the shield laws, allowing U.S.-based doctors to mail pills directly into antiabortion states instead of relying on international pharmacies. That change has reduced the shipment time from several weeks to between three and five days.
At the time Briana ordered her medication, over a year ago, Aid Access generally did not send pills to anyone who said they were further than 11 weeks into their pregnancy, Gomperts said. It now allows people to place orders through 12 weeks of pregnancy, because pills reach patients more quickly.
“If we think people might be longer than that, they get an email to make sure they can navigate the situation,” said Gomperts, who personally prescribed Briana’s medication, according to documentation reviewed by The Post. “Women have agency. They are perfectly capable of making these choices about their own health, and we are there to support them the best we can.”
According to data compiled by Aid Access, and shared with The Post, 1 in 20 patients who responded to the organization’s survey in January took the pills beyond 11 weeks of pregnancy. One in 100 took the pills beyond 13 weeks. (About 20 percent of people who took the pills responded to the survey.)
Still, Prine said, she has fielded far more of these calls from women later in pregnancy than she would like — averaging one a day on the hotline in the months after the Supreme Court decision. Some of the callers had no idea how far along they were until they passed the pregnancy, she said. Others knew, but chose to go ahead anyway.
Beyond 12 or 13 weeks, women will see a much more developed fetus, with identifiable features.
“We hear the trauma when we talk to people,” Prine said. “It’s an image you can’t get out of your head.”
Alone in her bathroom, Briana had no idea what to do. The Aid Access doctors had told her to expect nausea, vomiting, chills, blood clots and a fetus at least the size of an orange, emails show.
They said nothing about an umbilical cord.
“Do I pull the cord out?” Briana wondered, frantically trying to remember what the doctors had done when she gave birth. “Do I just wait to try to push it out?”
Her boyfriend was sleeping in the next room. Even if she woke him up, she wondered, what could he do? If she went to the emergency room, she said, she felt sure she’d be prosecuted.
Finally, Briana decided to call the number for the Miscarriage and Abortion Hotline she’d seen in an email from Aid Access.
“That’s the placenta you need to push out,” Briana recalled the woman on the hotline saying. “When you feel the next contraction, I want you to push like you’re giving birth.”
Briana said she sat there with her umbilical cord hanging loose for at least 15 minutes before the placenta finally dropped into the toilet.
While there are no major U.S.-based studies on the experience of self-managing an abortion with pills later in pregnancy, international research suggests that women in these situations more frequently seek in-person care. One study conducted with patients in Argentina, Nigeria and Southeast Asia between nine and 16 weeks of pregnancy found that about 24 percent went to a medical facility during or after the experience of taking the pills on their own. Approximately 10 percent required medical intervention to complete the abortion or treat a complication.
One major concern later in pregnancy is that the body won’t be able to expel all of the pregnancy tissue, several doctors said.
When the Miscarriage and Abortion Hotline received its first call from a woman who was unable to pass her placenta — at least five weeks further into her pregnancy than the FDA’s 10-week limit — a group of hotline doctors started messaging one another, trying to decide what to say to her, Prine said.
One doctor in the group insisted that the woman had to go straight to the ER, but Prine and others disagreed. Worried the woman could face prosecution or mistreatment if she went to the hospital, Prine said, they walked her through her abortion at home, instructing her to take more abortion pills and gently massage her stomach until the placenta came free — the same advice Briana said she received.
“We didn’t feel like it was a medical emergency. She wasn’t bleeding heavily and she wasn’t lightheaded,” said Prine, adding that they would have recommended the woman go the ER if a hospital visit was medically necessary.
A woman in that situation could have hemorrhaged or become septic, according to five OB/GYNs interviewed for this article.
“Whenever there is something inside the uterus that is trying to come out and won’t come out, the risk of bleeding and infection gets higher with every passing moment,” said Keri Garel, an OB/GYN at Boston Medical Center, adding that she would advise someone in Briana’s situation to go to the hospital immediately. “At that point, your life is the most important thing.”
“Do I pull the cord out?”
As difficult as the situation was, Briana says she is extremely grateful that Aid Access was willing to send her the pills — and that someone on the hotline was available to talk her through taking them.
“Without the hotline I would have been completely lost and literally completely alone,” she said.
“The lady … stayed talking to me for hours,” Briana added. “I wish I knew her name.”
Briana stayed in the bathroom that night for more than an hour. She knew she shouldn’t look at the fetus, she said, but she couldn’t help it. In the toilet bowl, she could make out a head. She remembered thinking that the legs looked long.
“I felt like a monster,” she said, reflecting back on that moment.
A year later, Briana said, she is certain she made the right decision for herself and her family. But she wishes someone had told her more about what to expect. If she had known the full extent of what could happen during a medication abortion at 15 or 16 weeks, she said, she probably would have searched harder for an out-of-state clinic with available appointments — and figured out a way to drive six hours or more to Florida, Illinois or North Carolina.
Before Roe v. Wade was overturned, Briana could have gone to a clinic less than 30 minutes from her house.
“We can see you tomorrow.”
“Here’s what you should expect.”
A former abortion provider offers some relief
“That website is real.”
“You are going to get through this.”
“Your uterus looks beautiful.”
In Houston, a woman lay back on an exam table in a clinic that once offered abortions, hoping to hear that her medication abortion was finally complete.
Ashley, a 25-year-old mother with a baby, opened her legs and stared up at a mermaid mobile hanging from the ceiling, her sweatpants and Converse sneakers in a heap on the floor.
“Are you ready?” Glenda Lima, the sonographer, asked on a Tuesday morning in mid-February. “There will be a little cold and just a little pressure, okay?”
It was Ashley’s fourth visit in two months to Houston Women’s Reproductive Services, one of a handful of former abortion clinics that have remained open in states with near-total abortion bans. While the staff originally imagined a new version of the clinic that offered ultrasounds and referrals to patients planning to travel out of state for medication and procedures, a large share of the women they serve are now self-managing their abortions with pills they got online.

As soon as she found out she was pregnant in mid-December, Ashley had ordered pills from Aid Access, which she’d heard about on TikTok. But the whole process seemed a little sketchy, she said. What kind of medical organization collected money through Venmo, she wondered? They were asking for a picture of her driver’s license. What if it was all a scam?
She decided that she needed to talk to someone. Not a disembodied voice on the phone or an anonymous commenter in an online forum — but a real, live person she could actually meet.
“If I’m putting this in my body,” Ashley recalled thinking to herself, “I need to know I’m going to be okay.”
Ashley struggled to come up with the right terms to Google, she said, wondering if it was even possible to get advice on abortions in a state where abortion is banned. She came across contact information for Houston Women’s Reproductive Services only after first messaging a crisis pregnancy center — an email thread she abandoned when she realized it was actually an antiabortion organization designed to dissuade women from ending their pregnancies.
Kathy Kleinfeld, the administrator of Houston Women’s, responded to Ashley’s panicked message on a Sunday, offering her an appointment for a pre-abortion ultrasound and consultation the next day the clinic was open.
“I was like, ‘Oh my God, I feel like I have been searching for this,’” Ashley said. For the first time since finding out she was pregnant, she said, “I just felt safe.”


As other Texas clinics moved to New Mexico and Illinois after Roe was overturned, Kleinfeld and Lima decided to downsize and stay put, anticipating that some women would continue to seek out ultrasounds, emotional support and general guidance in their home state, services that remain legal under Texas law. If all the abortion clinics shuttered, they said, they knew crisis pregnancy centers would be the only places left to go.
Now, the women see their clinic as a helpful counterpart to the online pill networks: a soothing space with a “relaxation” scented diffuser and three portraits of the late Supreme Court justice Ruth Bader Ginsburg, where Texans can get the help they need to feel comfortable self-managing their abortions at home.
There are major challenges to providing this kind of care in a state where abortion is illegal. Perhaps the biggest, Lima said, is that women assume there are no abortion resources left in Texas. Those that find them often do so by chance.
Lima said she regularly gets frantic calls and texts from Spanish-speaking patients she’s never met before on her cellphone, a number she gives out only to patients she sees in the clinic.
“I ask them, ‘How did you get my number?’” she said. “They say, ‘A friend of a friend of a friend.’”
“I need to know I’m going to be okay.”
Kleinfeld acknowledges that the very existence of a clinic like theirs — which, unlike some other former abortion clinics that have remained open in states with bans, has no doctors on site and offers no health services other than ultrasounds — is somewhat controversial in the abortion rights community. With abortion rights advocates arguing vehemently that in-person consultations and ultrasounds are entirely unnecessary for a medication abortion, Kleinfeld said, some likely see her clinic as an impediment to women accessing the care they need.
Kleinfeld would never want to see an in-person visit mandated for all patients — most women have no problem handling everything at home, she said. But she has learned that some need the additional hand-holding, especially when they are obtaining pills from unfamiliar sources.
“Not everybody needs an ultrasound, not everyone needs a phone number to call,” Kleinfeld said. “But some really do.”
Blair Cushing, a family medicine doctor who provided abortions in McAllen, Tex., before the clinic there was forced to close, recently opened a small medical practice near the Mexico border to offer ultrasounds and other support to women who self-manage their abortions. When she meets with patients, she said, they’ll often stay to talk for an hour or more — experiencing “information overwhelm” from everything they’ve read online and desperate for reassurance.
“They’re worried because something didn’t go the way they were expecting,” Cushing said. “They need to decompress about this experience they had and make sure they’re okay.”


Ashley first went to Houston Women’s Reproductive Services for an ultrasound before she took the pills on Dec. 19 — then returned a week later, wondering why she was still bleeding and experiencing a dull pain in her lower back.
Lima, the sonographer, told Ashley that she still had some blood clots left in her uterus. And while Lima assured her that this was nothing to worry about — the body can typically expel remaining clots without any medical intervention — Ashley wanted to be sure.
She returned to Houston Women’s for three more appointments, until Lima was able to confirm that all the clots were gone.
“Your uterus looks beautiful … nice and clean,” Lima said at Ashley’s final appointment in mid-February. “You’re good to go, okay?”
Ashley smiled, closing her eyes as she felt all the muscles in her shoulders finally relax.
“Thank you,” she said. “That’s all I needed to hear.”

About this story
Editing by Peter Wallsten. Photo editing by Natalia Jimenez. Copy editing by Thomas Heleba and Martha Murdock. Design editing by Madison Walls. Graphics editing by Emily M. Eng. Graphics reporting by N. Kirkpatrick. Design and development by Agnes Lee. Andrew Tran contributed to this report.